What is gout?
Gout is a painful form of arthritis caused by uric acid crystals that form in and around the joints.
It’s the most common type of inflammatory arthritis. It’s more common in men and you’re more likely to get it as you get older.
Gout occurs in people who have high levels of uric acid, also known as urate, in their blood. Urate is created every day when our bodies break down purines. Purines are chemicals that are naturally created in our body, but they are also present in certain foods.
We all have urate in our blood: this is normal and healthy. But if levels become too high it may cause gout.
People used to think that gout was caused by overeating and drinking too much alcohol. While this can make attacks of gout more likely, it’s not the whole story.
 On any day, about three-quarters of the urate in our bodies comes from the breakdown of purines produced within our body, while only about a quarter comes from food and drink. As urate levels build up, your body gets rid of any extra through your kidneys and in your wee. But if your body makes too much urate, or your kidneys are unable to get rid of enough of it, then levels start to rise.
On any day, about three-quarters of the urate in our bodies comes from the breakdown of purines produced within our body, while only about a quarter comes from food and drink. As urate levels build up, your body gets rid of any extra through your kidneys and in your wee. But if your body makes too much urate, or your kidneys are unable to get rid of enough of it, then levels start to rise.
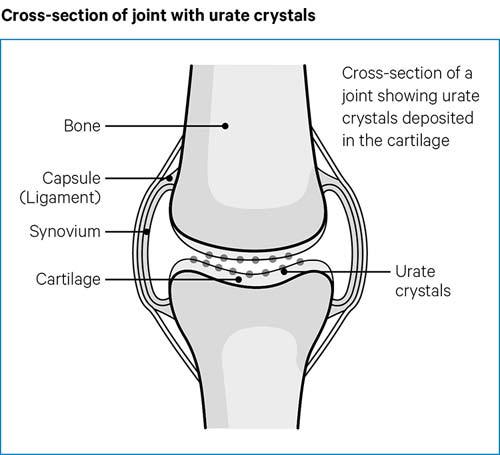
If urate levels stay too high, urate crystals can slowly form. They mainly occur in and around firm joint tissues, such as the cartilage. But crystals can also appear under your skin and may even occur in your internal organs, such as the kidneys.
What are the symptoms?
Symptoms of gout aren’t usually noticeable unless you are having an attack of gout. Attacks of gout usually last between five and seven days, where you will experience symptoms.
Attacks
When you have gout, urate crystals can build up in your joints for years without you knowing they are there. When there are a lot of crystals in your joints, some of them can spill out from the cartilage into the space between the two bones in a joint.
The tiny, hard, sharp crystals can rub against the soft lining of the joint, called the synovium, causing a lot of pain swelling and inflammation. When this happens, it’s known as an attack or flare of gout. A flare-up, or flare, is a period of time in which the symptoms of a condition come back or get worse.
During an attack of gout, the affected joint becomes:
- very painful
- tender
- red
- hot
- swollen.
The skin over the joint often appears shiny and it may peel off as the attack settles.
Attacks usually come on very quickly, often during the night. Doctors describe the sudden development of symptoms as ‘acute’.
The attack usually settles after about five to seven days, but it can go on for longer.
If gout is left untreated, attacks can become more common and may spread to new joints.
Attacks typically affect the joint at the base of the big toe and often start in the early hours of the morning.
The symptoms develop quickly. Usually, they feel worst within the first 12 to 24 hours of you noticing that anything is wrong.
Any light contact with the affected joint is very painful – even the weight of a bedsheet or wearing a sock can be unbearable.
Although gout most often affects the big toe, other joints may also be affected, including:
- other joints in your feet
- ankles
- knees
- elbows
- wrists
- fingers.
It’s possible for several joints to be affected at the same time. It’s not common to have gout in joints towards the centre of your body, such as the spine, shoulders or hips.
Gout attacks are especially common in joints at the ends of your legs and arms, such as in your fingers and toes. This may be because these parts of the body are cooler, and low temperatures make it more likely for crystals to form.
Similar attacks can be caused by a condition called acute calcium pyrophosphate crystal arthritis. This is also known as acute CPP crystal arthritis, which used to be called ‘pseudogout’. For more information see acute cpp crystal arthritis.
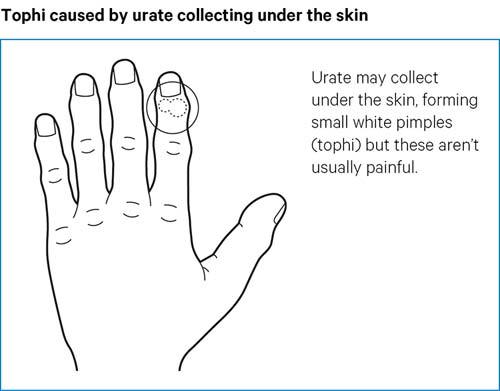
Tophi
Urate crystals can also collect outside of the joints and can be seen under the skin, forming small, firm lumps called tophi. You can sometimes see the white colour of the urate crystals under the skin.
The most common areas for tophi are:
- over the top of the toes
- back of the heel
- front of the knee
- backs of the fingers and wrists
- around the elbow
- the ears.
Tophi aren’t usually painful, but they can get in the way of normal daily activities. They can sometimes become inflamed, break down and leak fluid with gritty white material - these are the urate crystals.
Tophi can also grow within your joints and cause damage to your cartilage and bone. This can lead to more regular, daily pain when you use the affected joints.
How will it affect me?
Attacks can vary from person to person. Some people only have an attack every few years, while others may have attacks every few months.
Without medication, attacks tend to happen more often, and other joints can become affected. Having high urate levels and gout for a long time can lead to other health problems, including:
- narrowing of the arteries - which can lead to an increased risk of stroke, heart attacks or other heart problems
- osteoarthritis, which occurs when the urate crystals and hard tophi cause joint damage
- an increased risk of developing kidney disease or worsening of the condition if you already have it
- kidney stones
- an increased risk of some cancers, especially prostate cancer
- mental health problems, including depression
- underactive thyroid
- erectile dysfunction.
Most of the damage and complications caused by gout can be stopped if you take medication to lower your urate levels and have a healthy diet and lifestyle.
What causes gout?
There are two different types of gout. When you have it and there’s no single cause, it’s called primary gout. When you have it and it’s caused by something else, it’s known as secondary gout. Secondary gout can be caused by either:
- chronic kidney disease
- long-term use of medications that affect how well your kidneys can remove urate from your body.
Risk factors
There are a number of things which can increase your risk of developing gout.
Family history
Even though your kidneys can be completely healthy, sometimes the genes you’ve inherited make it more likely that your kidneys don’t flush urate out as well as they should.
This is the most common cause of primary gout, especially when several family members are affected, such as your parents or grandparents.
Being overweight
Gout is much more common in people who are overweight. The more overweight you are, the more urate your body produces. Your body may produce more urate than your kidneys can cope with.
Being overweight also makes it more likely that you’ll have:
- high blood pressure
- type 2 diabetes
- high cholesterol
- fats in your blood.
These conditions can all lower how much urate is filtered out by your kidneys.
Gender and age
Gout is about four times more common in men than women. It can affect men of any age, but the risk is greater as you get older.
Women rarely develop gout before the menopause. This is because the female hormone oestrogen increases how much urate is filtered out by the kidneys. But after the menopause, oestrogen levels go down and urate levels go up.
The menopause is a natural part of ageing, and usually happens in women aged between 45 and 55. It's when a woman stops having periods and is no longer able to get pregnant naturally. Find out more about the menopause.
Taking certain medications
Some medications can reduce your kidneys’ ability to get rid of urate properly. These include diuretics, also known as water tablets, and several tablets for high blood pressure, including beta-blockers and ACE inhibitors.
If you are on these, you should speak to your doctor about the risks if you are concerned.
Other conditions
Several different conditions are linked to raised urate levels. This could be because they affect the way the kidneys filter urate, or because they cause more urate to be produced in the first place.
For some conditions, the link with gout is less clear and may be due to many different factors.
Common conditions associated with gout include:
- chronic kidney disease
- high cholesterol and fats in the blood
- high blood pressure
- type 2 diabetes
- osteoarthritis.
What can trigger an attack?
Several things can cause the crystals to shake loose into your joint cavity, triggering an attack. These include:
- a knock or injury to the joint
- an illness that gives you a fever
- having an operation
- having an unusually large meal, especially a fatty meal
- drinking too much alcohol
- dehydration
- starting urate lowering therapy (ULT), especially at a high dose, or not taking your ULT regularly each day.
Diagnosis
Diagnosing gout is usually straightforward, especially if you have typical symptoms of the condition. For example, if you have an attack in your big toe.
But gout can sometimes be more difficult to diagnose. Your doctor will need to know about the symptoms you’ve been having and will probably need to do some tests.
Blood tests
Blood tests to measure your urate levels can be helpful to support a diagnosis of gout. But they aren’t enough to confirm it on their own.
High urate levels in blood tests can suggest that you have gout. But this will need to be considered alongside your symptoms. It’s possible to have high levels of urate, but not have any other symptoms of the condition.
Scans
Ultrasound and CT scans can be good at spotting joint damage, crystals in the joints and early signs of gout.
X-rays are generally used to pick up the bone and joint damage caused by having gout for a long time.
Synovial fluid test
This is a good way to confirm the diagnosis and rule out other causes.
This examination is done by taking a sample of your synovial fluid. Synovial fluid is made inside the capsules of some joints. It helps to nourish and lubricate the joints.
This is done by inserting a needle into one of your joints. The fluid is then examined under a microscope for urate crystals. If you have tophi, doctors can take a sample from one of those instead.
Treatments
Treatments for gout can be very successful. There are two main parts to treating gout which include:
- treating the acute attack
- treatments to prevent future attacks.
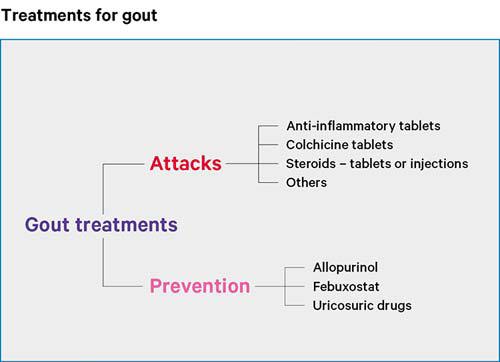
Treating a gout attack
Treating an attack of gout doesn’t lower your urate levels or stop future attacks. The treatment helps you to manage your symptoms when an attack happens.
The most common drug treatments for attacks of gout are:
Some people will be better suited to NSAIDS, while for others NSAIDs cannot be used. But your preference is also taken into consideration. Many people with gout quickly learn what works best for them.
In cases where one drug doesn’t seem to be working on its own, your doctor might suggest a combination of NSAIDs with either colchicine or steroids.
Non-steroidal anti-inflammatory drugs (NSAIDs)
Attacks of gout are often treated with NSAID tablets, which can help with pain and reduce some of your inflammation. Naproxen, diclofenac, and etoricoxib are three NSAIDs you could be given.
If you’ve been prescribed NSAIDs to treat an attack, you should start taking them as soon as you notice signs of one coming on. Your doctor may let you keep a supply so you can start taking them at the first signs of an attack.
The earlier you start treatment, the better.
NSAIDs aren’t suitable for everyone, so talk to your doctor about them first if you have any other conditions. They can also interact with other drugs, so make sure you talk to a doctor before starting on any new medication.
NSAIDs aren’t usually prescribed for a long period of time, as they can cause problems with your digestive system. To reduce the risk of this happening and to protect your stomach, your doctor will also prescribe a proton pump inhibitor.
Colchicine
Colchicine isn’t a painkiller. But can be very effective at reducing the inflammation caused by urate crystals.
As with NSAIDs, colchicine tablets should be taken as soon as you notice an attack coming on, or it may not work as well. Your doctor will probably recommend keeping a supply at home.
Colchicine can interact with several other drugs, including statins taken for high cholesterol. Your doctor will advise whether you’d be better off taking an NSAID instead or adjusting your other medications while you’re taking colchicine.
You should avoid taking colchicine if you have chronic kidney disease.
Colchicine tablets can cause diarrhoea or stomach aches.
Steroids
Steroids are very useful for acute attacks of gout.
They are usually taken as a short course of tablets, lasting a few days.
However, they can also be taken as an injection into a muscle or joint affected by gout. This can be particularly helpful if gout is affecting only one joint.
Tips for managing an attack at home
- Keep the area cool – an ice pack, or a bag of frozen peas wrapped in a tea towel, can be particularly good at reducing some of the pain and swelling.
- Rest the affected joint.
- Think about getting yourself a bed cage. These support the bedsheets above your feet so that your affected joint can rest without the strain of the sheets.
Treatments to prevent gout attacks
There are drugs available that can lower urate levels, prevent new crystals from forming and dissolve away the crystals in your joints. They are called urate lowering therapies (ULTs).
Treatment with ULTs is generally started after an attack of gout has completely gone.
There’s no single fixed dose of a ULT, and different people need different doses to get to the right blood urate level.
It can take a few months or years for the drugs to completely clear your body of urate crystals. But once they’re gone, you will no longer have attacks of gout, tophi or risk of joint damage due to gout.
It’s important to remember that ULTs won’t stop attacks of gout straight away. You might have more attacks within the first six months of starting them.
Don’t stop taking your ULTs if this happens to you, as this is actually a sign that the drugs are working. As the drugs start dissolving the crystals, they become smaller and are more likely to get into the joint cavity, triggering an attack.
Your doctor might suggest taking a low dose of colchicine or NSAID as a precaution against attacks during the first six months of starting ULTs.
ULTs are usually life-long treatments and require yearly check-ups to monitor your urate levels. If your symptoms aren’t getting under control, talk to your doctor about your urate level, as you might need to be on a higher dose.
Try not to miss or skip any of your doses, especially in the first year or two of starting treatment. This could cause your urate levels to go up and down, which could trigger an attack.
Allopurinol
Allopurinol is the most commonly used ULT. It’s a very effective treatment for most people with gout.
It works by reducing the amount of urate that your body makes.
You’ll start on a low dose of allopurinol, which can be gradually increased until you are on the right dose.
Gradually building up the dose means it’s less likely to trigger an attack. It also makes sure that you have the lowest dose needed to get your gout under control.
Allopurinol is broken down and removed from the body through your kidneys, so if you have a problem with your kidneys, it may not be suitable for you.
Your doctor might decide to start you on a very low dose and increase slowly or suggest that you try febuxostat instead.
Allopurinol won’t be given to you if you are currently having an attack of gout or are sensitive to allopurinol.
Febuxostat
Febuxostat is a newer drug that reduces the amount of urate made in the body in the same way that allopurinol does.
You won’t be prescribed febuxostat as your first ULT, unless your doctor has said that you can’t take allopurinol.
It works in a similar way to allopurinol but, instead of being broken down by the kidneys, it’s broken down by your liver. It’s useful if you have kidney problems and can’t take a high enough dose of allopurinol.
Febuxostat is more likely to trigger gout attacks than allopurinol when you first start treatment. So, as a precaution, it’s likely you’ll be prescribed a low-dose NSAID or colchicine to take for the first six months of taking febuxostat.
There are just two doses of febuxostat, so if your urate levels haven’t lowered enough after a month on the low dose, you may need to go on to the higher dose.
Uricosuric drugs
Uricosuric drugs, which include sulfinpyrazone, benzbromarone and probenecid, work by flushing out more urate than normal through your kidneys.
They’re not used much in the UK, as they’re not widely available. They’ll only be prescribed by a rheumatologist if allopurinol and febuxostat haven’t worked or aren’t suitable for you.
It’s unlikely you’ll be able to take these drugs if you have severe problems with your kidneys or kidney stones. This is because uricosuric drugs encourage your kidneys to filter more urate. In doing so, it also increases your risk of developing kidney stones.
Uricosuric drugs are usually prescribed on their own. But in rare cases, where you’ve tried several ULTs and none have worked for you, uricosurics can be used along with other ULTs, like allopurinol or febuxostat.
If you’re unable to take allopurinol, febuxostat or a uricosuric drug, or if they don’t work for you, you’ll need to see a rheumatologist for advice.
Treatment for joint damage
If gout has caused damage to your joints, then treatment will be similar to that for osteoarthritis. It includes:
- exercising regularly
- reducing the strain on your affected joints
- staying at a healthy weight
- taking painkillers
- in more severe cases, joint replacement surgery.
Find out more information about joint damage by viewing our osteoarthritis section.
Malcolm's story: improving treatment for gout
Managing symptoms
Lifestyle choices are not the main reason why most people get gout.
But, if you have a healthy lifestyle and take prescribed medication, you’ll have the best chance of lowering your urate levels. This will then decrease the chances of you having attacks of gout.
Keeping active
Staying active is not only important for your general health and wellbeing, but it also reduces your chances of having a gout attack.
It doesn’t matter how much exercise you do - a little is better than none at all.
Start off slowly and gradually build up how much you do until you’re doing regular sessions.
As your confidence increases, you can increase the length and intensity of what you’re doing.
Exercise that leaves you out of breath is particularly good. You could try dancing, walking across hilly countryside or tennis.
It helps to find a sport or exercise that you enjoy and will keep doing. Some people find joining a leisure centre or sports club really motivational. Have a look around and see what’s available in your area.
You should avoid exercising during a flare-up of gout, as it could make your pain worse. It’s important to rest and recover and begin exercising after the pain and swelling have gone down.
More information on exercise and arthritis.
Healthy eating
You should try to eat a balanced diet that is low in fats and added sugars, but high in vegetables and fibre.
Keeping to a healthy weight is important for your general health and wellbeing, but it can also help if you have gout. This is because being overweight can put more strain on your joints.
If you’re overweight, you should try to lose weight gradually by eating a balanced diet and keeping active.
Extreme weight loss or starvation diets aren’t recommended because these can raise urate levels. However, you should be OK to do some daytime fasting - for example, during Ramadan.
Atkins-type weight-loss diets aren’t recommended, as they include a lot of meat and are high in purines.
The NHS has a good diet and exercise plan which can help you lose weight in a healthy way over 12 weeks. Find out more on the NHS website.
Food to have in moderation
The food and drink you consume can increase the amount of uric acid in your body.
Some foods can be worse for you than others, but you shouldn’t have to remove anything completely from your diet.
You should try to avoid eating large quantities of:
- red meat, game and offal - such as venison, kidneys, rabbit and liver
- seafood, particularly oily fish and shellfish - such as anchovies, fish roe, herring, mussels, crab and sardines
- foods rich in yeast extracts - such as Marmite, Bovril and Vegemite
- processed foods and drinks.
Protein is an important part of your diet, but you can get it from sources other than meat and fish. You could try replacing a portion of meat with other protein-rich foods like soybeans, eggs, pulses or dairy products.
The UK Gout Society has a detailed food list of foods high in purines. Check out their diet factsheet for more information.
What about drink?
If you have gout and a history of kidney stones, you should try to drink at least two litres of water a day to decrease the chance of stones forming.
Try to avoid sweetened soft drinks because they contain large amounts of sugar and can increase your risk of gout.
While fruit and fresh fruit juices contain sugar, the benefits of eating fruit far outweigh any negatives. Reducing how much sugar you consume from other sources is a healthier option than cutting out some of your five a day.
Alcohol
Drinking too much alcohol, especially beer and spirits, can increase your urate levels and your chances of triggering a gout attack. Beer is particularly bad, as it contains a lot of purines.
However, drinking small amounts of wine doesn’t appear to increase the risk of triggering an attack.
As a rule of thumb, try to stick to the government guidelines of drinking no more than 14 units a week. This is equivalent to about 6 pints of beer or 6 glasses of wine. But don’t save these units up and drink them all in one go - it’s better to spread them out over the course of the week.
Your doctor might also advise a lower limit.
Find out more on the drinking guidelines on the drinkaware website.
Vitamin C
Research has shown that vitamin C may slightly reduce uric acid levels in people with gout. This is another reason to make sure your diet includes plenty of fruit and vegetables.
But if you’re considering taking vitamin C supplements, talk to your doctor first, as there’s a very slight risk that vitamin C supplements could interact with other medications.
Cherries
Research has shown that cherries may reduce the risk of having an acute attack of gout, particularly when taken with allopurinol.
Skimmed milk and low-fat yoghurt
Research suggests drinking skimmed milk and eating low-fat yoghurt may help to prevent attacks of gout.
Complementary and alternative treatments
Don’t use complementary treatments, such as herbal remedies, without discussing this first with your doctor or pharmacist as some of them could react with your prescribed gout medication.
If you decide to try complementary and alternative treatments, you should be critical of whether they are making a difference to your condition.
They should never replace your prescribed gout medication.
Don’t worry about fish oil supplements raising your urate levels. While some may contain purines, the amount is likely to be so small that it won’t make a difference to your condition.
Similarly, even though the supplement glucosamine is made from the outer shells of shellfish, it doesn’t contain purines. However, there’s no evidence that glucosamine can prevent or treat gout.
Living with gout
Work
Work can provide a sense of purpose, a supportive social network, and help you financially.
Most people with gout can continue working, but you may need some time off when you have an attack.
If gout is affecting your ability to work, speak to your employer’s occupational health service if they have one. Your employer has a duty to make reasonable adjustments so that you can do your job.
Your local Jobcentre Plus can also put you in touch with Disability Employment Advisors, who can arrange workplace assessments.
If your employer can’t make all the adjustments you need, you may be able to get help through Access to Work. This can cover grants to pay for equipment or adaptations, support workers to help you, or help to get to and from work.
Access to Work operates in England, Scotland, Wales and Northern Ireland. But the application process differs from place to place.
Learn more about working with arthritis.
Emotional wellbeing
The emotional effects of gout can have just as much impact as the physical symptoms.
Long-term damage and severe pain from the attacks of gout can affect your daily life, disturb your sleep, and affect your mood.
From time to time, your gout may get on top of you. If you’re feeling low, talk to your GP, who can signpost you to the appropriate services.
There are also plenty of small ways you can look after your mental wellbeing and build emotional resilience. For instance, you could:
- Practice deep breathing or mindful meditation to help reduce any anxiety you may have.
- Write your thoughts down in a diary to help you make sense of your emotions.
- Keep active – exercise can give you a boost of feel-good hormones called endorphins.
- Make time for activities that you enjoy, or which help you relax.
- Connect with friends – grab a coffee with a friend, have a phone call with a family member or join an online community.
You can also call our helpline on 0800 5200 520, who can listen and offer emotional support.
Sleep and fatigue
Gout attacks can tend to occur at night. This can cause you to have trouble sleeping. During attacks you may also feel fatigued.
If a gout attack occurs during the night it may be helpful to:
- raise the affected joint on a cushion
- put ice on the joint
- take any medication that your doctor has recommended
- try and not let any bed sheets touch the affected joint as this can make the pain worse.
A change in habits around your bedtime may also help improve your sleep:
- Make sure your bedroom is dark, quiet and a comfortable temperature.
- Try a warm bath before bedtime to help ease pain and stiffness.
- Develop a regular routine, where you go to bed and get up at a similar time each day.
- You may like to try listening to some soothing music before going to bed.
- Some gentle exercises may help reduce muscle tension, but it’s probably best to avoid energetic exercise too close to bedtime.
- Keep a notepad by your bed – if you think of something you need to do the next day, write it down and then put it out of your mind.
- Avoid caffeine in the eight hours before you go to bed.
- Don’t drink alcohol close to bedtime.
- Avoid eating main meals close to bedtime.
- If you smoke, try to stop smoking, or at least don’t smoke close to bedtime.
- Try not to sleep during the day.
- Avoid watching TV and using computers, tablets or smartphones in your bedroom.
- Don’t keep checking the time during the night.
Neil’s story

At its worst I couldn’t walk for three months, I couldn’t drive, I couldn’t even play with my daughter.
My gout started when I was only a year into my thirties and the only way that I could get around was by crawling on all fours.
When I was initially diagnosed, my doctor gave me the impression that having gout was my fault. He just prescribed me ibuprofen and told me to change my diet.
He even said that drugs like allopurinol would be “bad for my guts” and I would be better off without them.
Taking on his advice, I didn’t drink any alcohol for 14 years. I also changed my diet, avoiding and eating less of the foods that can make gout worse.
But nothing changed. The pain was excruciating. My gout had now spread to my elbows, wrists, hands, and fingers.
When I went to my doctor with all this new pain, he thought I had arthritis, so I was referred to a rheumatologist.
The rheumatologist was fantastic and took one look at my urate levels and knew it was gout that had spread. She was appalled I had never been prescribed allopurinol before, so started me on it right away.
The next six years of my life were fantastic, I had no problems at all. I didn’t have to worry as much about my diet and my gout was under control. It was miraculous.
I had even started exercising regularly doing a range of bike, low impact and resistance band workouts.
Then in 2020, a rash appeared all over my body apart from my neck and head. It wasn’t itchy but it was very prominent. It looked like I had chickenpox or rubella.
After some blood tests I was told I had developed an allergy to allopurinol, and I had to stop taking the drug.
It was hard to process. It was such a shock to me, and it was scary having to stop taking it as I didn’t want my gout to return.
Luckily enough it didn’t. I always keep a strong painkiller beside me and, since 2017, I have lost seven stone, which has been great for my health and has helped with my gout.
If you have gout, my advice would be don’t panic, do your research, and find out everything you can. And if you’re not getting the help you need, go somewhere else. You can always find someone who’ll help.