What is osteoarthritis of the elbow and shoulder?
Osteoarthritis is the most common form of arthritis. It can affect any joint in your body, but the elbows and shoulders are less commonly affected than other joints.
Everyone’s joints go through a normal cycle of wear and repair during their lifetime. As your joints repair themselves, their shape and structure can change. When this happens in one or more of your joints, it’s known as osteoarthritis.
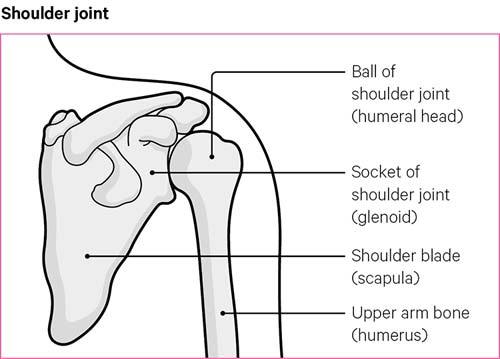
A joint is a part of the body where two or more bones meet. The shoulder joint is known as a ball and socket joint. It’s called this because the top of your upper arm bone is shaped like a ball. This fits into your shoulder blade bone, which acts like a socket. This gives your shoulder a wide range of movement.
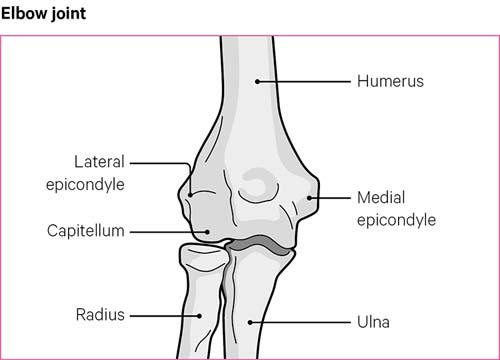
The elbow joint connects the upper arm bone, which is called the humerus, with the bones in your forearm, called the radius and ulnar.
The elbow is known as a hinge joint because your elbow allows you to bend and straighten your arm. It also allows you to rotate your forearm and wrist.
The ends of both bones in a joint are covered by a smooth, slippery surface, known as cartilage. This is the soft but tough tissue that allows your bones to move against each other without friction.
Osteoarthritis causes the cartilage in your joints to become thinner, and the surfaces of the joint to become rougher, as new layers of bone begin to grow.
The exact cause of osteoarthritis is often not known, as there can be quite a few reasons why a person develops the condition. These include the genes inherited from your parents.
Osteoarthritis is common and can affect people of any age, but it usually starts in people over the age of 45.
Research has shown that injuries and jobs that put repeated strain on your elbows and shoulders can increase your risk of getting osteoarthritis in these joints.
How will osteoarthritis of the elbow and shoulder affect me?
While many people with osteoarthritis of the shoulder or elbow won’t have any symptoms, those who do can have a wide range of experiences.
Most commonly the affected joint can feel stiff, swollen and painful.
But being diagnosed with osteoarthritis doesn’t mean your condition will get worse. There’s a lot you can do to improve your symptoms. See the section ‘managing osteoarthritis’ to find out more.
Osteoarthritis won’t always affect both of your elbows or shoulders. It may only affect one joint.
You might find it difficult to bend or stretch your arm, and you may feel pain when you move your shoulder. This could mean that simple activities like shaving or brushing your hair can suddenly become much more difficult.
You might hear some crunching or crackling noises, especially when moving your shoulder. But this usually isn’t anything to worry about and only sounds loud because this joint is close to your ears.
The pain may feel worse at the end of the day, or when you move your arm, and it may improve when you rest. You might feel a bit stiff in the morning, but this shouldn’t last more than half an hour.
Complications
It’s unlikely that osteoarthritis of the elbow or shoulder will cause you any serious complications. But in some cases, damage and swelling of the joint could put pressure on nearby nerves.
If this happens in your elbow, it could cause numbness or tingling in your little or ring fingers. You should mention these symptoms to your doctor, as there are things they can do to help.
In some cases, surgery may be needed to relieve the pressure on the nerves and treat your symptoms.
Managing osteoarthritis of the elbow and shoulder
There are many treatments that could significantly reduce your pain and improve your movement. You’ll probably need to use a combination of things to get the best results.
You should discuss the following treatments with your doctor, so that you can be involved in picking the right treatment plan for you.
Exercise
Whatever your fitness level, exercise or any kind of regular physical activity should form a core part of your treatment. Here are some exercises for the elbows and shoulders that you may want to try.
It’s important to keep moving, as this will help reduce the pain and fatigue caused by your osteoarthritis. It may also help your sleep.
Many people with joint pain worry that moving more might make things worse, but this isn’t true. Keeping your muscles and bones strong will support your joints and make you feel better.
Try to start off slowly and gradually increase how much you do. Exercising little and often is a good place to start.
There are three different types of physical activity that are good for osteoarthritis and general health:
- Range of movement exercises, also called stretching exercises, help improve movement and maintain the flexibility of your joints.
- Strengthening exercises will build up your muscle strength around your joints, so they are better supported and more stable.
- Aerobic exercises are important for your health and fitness, especially for your heart.
You should try to do at least 20 minutes exercise each day, building up to at least 150 minutes of moderate aerobic activity every week and doing strengthening exercises on two or more days a week.
You might have to avoid forms of exercise that put too much weight on your elbows and shoulders, such as those that involve heavy lifting.
Swimming can be a great exercise to try, as it increases muscle strength.
The best exercise is something you’ll enjoy and keep doing. Try a number of different things, maybe even join a class, and see what works best for you.
Aqua aerobics, T’ai chi and Pilates are great if you want to improve your strength and range of movement.
If you’re worried about starting new types of exercise, speak to a physiotherapist. They’ll be able to give you tailored advice and start you on a personalised exercise plan. You can sometimes be referred to a physiotherapist on the NHS, but the waiting times might be quite long. Speak to your doctor for more details.
Sometimes your GP can refer you to a supervised exercise programme at a gym. Mention this to your doctor and see what’s available in your area.
Diet
Keeping to a healthy weight is good for all your joints, including your elbows and shoulders.
There’s no specific diet that’s recommended for people with osteoarthritis. However, if you need to lose weight, try to follow a balanced, reduced-calorie diet, combined with regular exercise.
The NHS has a great weight loss plan that can help you lose weight in a healthy way.
You can also speak to your doctor for advice. The Association of UK Dieticians also has an informative leaflet on diet and OA.
Reducing the strain
Generally, it’s best to carry on with your normal activities as much as you can – but don’t overdo it. You may need to pace yourself more than usual and try to gradually do a bit more each day.
You should avoid carrying heavy or bulky items with your affected arm or shoulder.
Having bad posture can also make your pain worse. So, make sure you’re sitting comfortably and changing your position often at home or at work. Take frequent breaks from sitting and gently stretch your shoulders and arms.
When working at a desk adjust your chair height, so that your arms and wrists are straight, making an L shape at the elbow. You can use a wrist rest to keep your hands level with the keyboard.
You might want to consider making changes to your home, car or workplace to reduce unnecessary strain.
An occupational therapist can advise you on special equipment, like dressing aids, which can make everyday tasks much easier.
Coping with low mood and sleep problems
You might find that osteoarthritis makes you feel depressed or anxious. Speak to your doctor if you’re feeling low. They may suggest cognitive behavioural therapy (CBT) and a few stress-relieving techniques.
The NHS also offer counselling sessions if you’re living with chronic pain or long-term health conditions.
Osteoarthritis can also affect your sleep pattern. This can lead to tiredness and could make your pain feel worse. You may even have fatigue, which is when you feel extremely tired, even after resting.
But there are things you can do for yourself that might help, such as:
- Avoid lying on the side of the affected arm. Instead lie on your back with a pillow supporting your arm.
- Keep a sleep diary to work out if there are any patterns to your sleep problems.
- Sleep at regular times to get your body into a routine.
- Avoid using mobile phones, laptops or computers in bed.
- Try to wind down before bed by having a warm bath or reading a book.
Your condition can affect your relationships and how you interact with people generally. It might be worth having conversations with people close to you to explain your condition and how it affects you.
If you’re still having problems, speak to your doctor or an occupational therapist. They can give you some tips and techniques and may also refer you to a pain management clinic, where you can be shown how to live a more active life.
Drugs
Drugs can be used to help ease the pain and stiffness caused by osteoarthritis. You’ll have the best results if you keep active, reduce the strain on your arms, and take medication that works for you.
Some of the drug treatments you may be recommended include:
- Painkillers: over-the-counter painkillers such as paracetamol may help, but your doctor may prescribe you stronger painkillers if needed.
- Non-steroidal anti-inflammatory drugs (NSAIDs): a short course of NSAIDs, such as ibuprofen, can help reduce pain, inflammation and swelling. However, NSAIDs aren’t suitable for everybody, so make sure you speak to a pharmacist before taking them.
- Steroid injections: an injection into the elbow or shoulder joint, which can help reduce your pain. Usually you’ll only be able to have three of these a year.
If you’re taking any of the over-the-counter medications mentioned above, make sure you’re using them as directed by your doctor or the patient information leaflet. Make sure whoever is treating you knows all the medication you’re taking.
Other pain relief
You might also want to try some of the following to help with your pain:
- Transcutaneous electrical nerve stimulation (TENS): this is a small machine that sends tiny electric shocks, through pads placed on your skin, to relieve pain. TENS machines aren’t suitable for everyone, so talk to your doctor before using one.
- Heat therapy: ice packs and heat packs, such as a hot water bottle or a bag of frozen peas, can relieve some of the pain and stiffness in your elbows and shoulders. Be careful not to put ice or heat packs directly on your skin, as they could cause burns. Make sure to wrap them in a damp tea towel or cloth.
- Hyaluronic acid injections: hyaluronic acid occurs naturally in the body and helps to lubricate joints. These injections are unlikely to be available on the NHS, as they’ve not been proven to be an effective treatment for osteoarthritis.
- Supplements: there’s a wide range available, including fish oils, turmeric, glucosamine and chondroitin. There’s very little evidence on how well they work, but some people with osteoarthritis do find them helpful.
- Acupuncture: is a technique where very fine needles are inserted at specific points in your skin. There’s no evidence that acupuncture is an effective treatment for osteoarthritis, but some people find that it helps them.
You need to be wary of some of these treatments, but what works for you can be completely different to what works for someone else. If you think some of these treatments could be right for you just have a quick chat with your doctor first.
Surgery
There are many treatments and exercises you can try to reduce the effects of osteoarthritis. But if these don’t work, and your pain is affecting your quality of life, you might benefit from surgery.
Shoulder and elbow joint replacements are very successful. However, you should expect it to take several months before you feel the full effects.
Before having surgery, you’ll be involved in a shared decision-making process. This involves discussing the best options for treating your condition and covers the risks and benefits of surgery.
The process is usually carried out by a surgeon or an advanced physiotherapist practitioner. They can give you the best advice and information, so you can make the decision that’s right for you.
Related information
-
Let's Move with Leon
Sign up to Let’s Move with Leon our weekly email programme of 30-minute movement sessions, presented by fitness expert Leon Wormley.
-
Let's Move
Sign up to Let’s Move to receive a wide range of content about moving with arthritis – from exercise videos to stories and interviews with experts – straight to your email inbox.