Plantar fasciitis
What is plantar fasciitis?
Plantar fasciitis affects the bottom of the foot, most commonly causing pain in the centre and inner side of the heel.
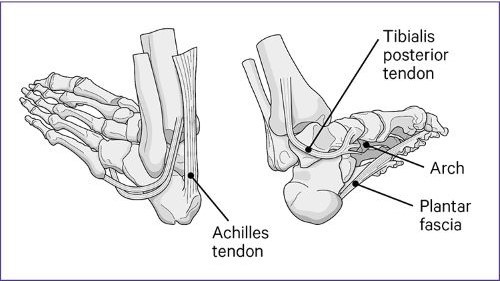
It's caused by damage to the strong band of tissue, called the plantar fascia, which runs from the heel, beneath the arch of the foot to the base of the toes.
Usually, the plantar fascia supports the arch and helps the foot work properly, spreading your weight evenly through your foot, so you can walk, run or stand without difficulty.
However, plantar fasciitis can make it difficult and painful to use your foot properly, particularly just after you have been resting. You may find the pain improves when your foot is active, for example during exercise, but returns soon after you stop.
Plantar fasciitis can be caused by:
- a sudden increase in the amount of activity you do
- being on your feet for too long
- exercising on hard surfaces
- overstretching the sole of your foot
- being overweight, as it increases the strain on your heels
- an injury or weakness in the ankle
- high or low arches
- ageing, as it is more common in people over 40
- shoes that do not cushion or support the soles of your feet
- tightness in the calf.
Plantar fasciitis can increase the risk of lumps of calcium collecting on the heel bone, called bone spurs, which can make your pain worse.
Weakness in the plantar fascia can also put additional strain on your ankle and knee.
How can I treat plantar fasciitis?
Plantar fasciitis can often be treated without the need to see a healthcare professional.
Paracetamol and ibuprofen can help reduce your pain.
There are some simple self-care tips, known as RICE therapy, that should help it heal:
- Rest – try to avoid putting weight on your heel. Do not exercise, instead try gently moving it from time to time to stop the area getting stiff.
- Ice – put an ice pack or frozen vegetables, covered in a damp cloth, on it for 20 minutes every 2–3 hours.
- Compression – wrap a bandage around the painful area. It should be tight enough to support it, but not so tight that it restricts the blood flow.
- Elevate your foot to reduce swelling.
When it's painful, rolling a cold drink can over the base of your foot for about 20 minutes should help. Gently massaging and stretching your calf, ankle and foot when you're resting can also make it easier to get moving again.
You can reduce the pressure on the bottom of your foot by wearing wide-fitting, comfortable shoes with a supportive sole and cushioned insole. They should fasten with a lace or strap and have a heel that is slightly raised by about 2–3cm, such as a good sports shoe.
Try to avoid walking on hard surfaces with bare feet, wearing tight pointy shoes, high-heels, backless slippers, flip-flops, or flat shoes.
Ask your pharmacist about insoles, heel pads and other pain relief. There is no proof that costly magnetic insoles are any better than regular cushioned insoles.
It can take up to 18 months to fully recover from plantar fasciitis. However, if you feel these self-management tips have not helped after two weeks, seek advice from your doctor, a physiotherapist or a podiatrist.
They may recommend:
- specially made insoles or foot supports
- stronger pain relief
- steroid injections in extreme cases
- additional medication to help reduce any inflammation.
Over the long term try to follow a healthy diet. If you are overweight, research shows that reducing the strain on the plantar fascia by losing even a small amount of weight can improve your pain levels.
You can find exercises for plantar fasciitis on our foot and ankle pain page.