What is Sjögren disease?
Sjögren (pronounced show-grin) disease is an autoimmune condition. This means that the immune system, which is the body’s natural self-defence system, gets confused and starts to attack your body’s healthy tissues.
Inflammation is your body’s normal reaction to injury or infection. You might notice inflammation if you have a cut or a wound. It causes the affected area to hurt and turn red. It may also become hot, as fluid rushes to the area and causes swelling.
The inflammation seen in Sjögren disease particularly affects the glands in your body that produce tears and saliva. This causes your eyes and mouth to become dry. Other parts of the body can also be affected, leading to dryness of the:
- skin
- throat
- breathing tubes
- gut
- vagina.
There are two types of Sjögren disease. When you have it on its own, it’s known as primary Sjögren disease. When you have it and it’s linked to another condition it’s known as secondary Sjögren disease. People with secondary Sjögren disease may already have other conditions such as rheumatoid arthritis, lupus or systemic sclerosis.
“It was hard to be diagnosed with Sjögren disease. It is so rare, and I really didn’t know anything about the condition. I thought I was just going to a routine rheumatology appointment for my rheumatoid arthritis and I was diagnosed with another condition.”
Symptoms
The most common symptoms are:
- dry eyes
- a dry mouth
- feeling tired and achy.
Many people who have the condition don’t have any other symptoms. However, symptoms can vary a lot from person to person. Some people find they can manage their condition well, while others find it has a big effect on their daily life.
Eye problems
Your eyes may be dry and feel sore, irritable or as if they have grit or sand in them. Some people feel discomfort under strong lights, or find their eyes become sticky with mucus.
Sometimes the eyelids might be sore or swollen, or your vision might become blurred.
Mouth and throat problems
Your mouth may be dry and you may get mouth ulcers. Your mouth or throat might also feel sticky.
It can sometimes be hard to swallow, or you might find that things taste different. You may find that you need to drink water while eating. Your voice may be hoarse or weak, and some people have a dry cough.
You could also have cracks in the skin at the corners of your mouth, or your tongue might look red and smooth.
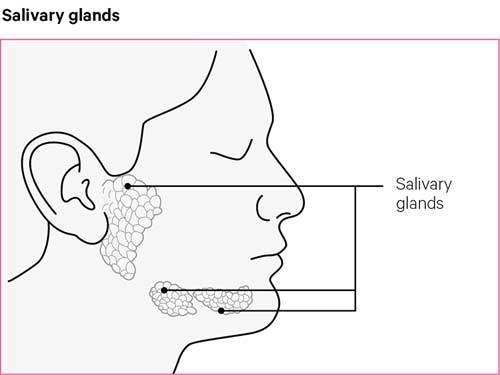
Occasionally, a very dry mouth can lead to other problems. These include fungal infections such as thrush, an unpleasant taste in your mouth, and more tooth decay. Your salivary glands, which are on your face, just in front of your ears, may feel painful and swollen.
Fatigue
Fatigue is an overwhelming feeling of tiredness that can happen after doing very little and has no obvious cause. You may feel extremely tired, both physically and mentally, and you might find it difficult to concentrate.
Some people start to feel down or depressed as a result of their condition and the fatigue it causes.
Aches and pains
Your joints may be painful and swollen due to inflammation, or you might feel that various parts of your body, such as your muscles, are achy and tender. Some people with this condition have headaches and migraines.
Other symptoms
You may feel as though other parts of the body are drier than normal, such as:
- your bowel – this may cause symptoms similar to irritable bowel syndrome (IBS), such as tummy pain, diarrhoea and constipation
- your bladder – this may cause irritation, soreness, or the need to pee more than usual
- your vagina – this can make sex uncomfortable and could cause symptoms of the menopause to feel worse
- your skin – this can make you feel itchy or unusually sensitive to strong sunlight. You might also get rashes
- your air passages – this may make you more sensitive to things in the air, such as smoke or dust, and cause a dry cough.
Who gets Sjögren disease?
Women aged between 40 and 60 are most likely to be diagnosed with Sjögren disease but it can affect anyone. Only about 1 in 10 people with the condition are men.
Causes
In Sjögren disease, the body’s immune system produces inflammation that damages the tissues and nerve signals to certain glands in the body.
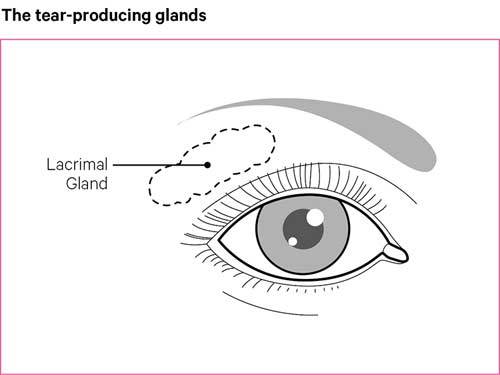
The inflammation mainly attacks glands that produce fluids, such as the lacrimal glands behind the eyelids, and the salivary glands in the mouth. This reduces the amount of saliva, tears and other fluids the glands produce.
We don’t know what causes the immune system to start attacking the body, but it’s thought it could be partly due to the genes we inherit from our parents. However, this doesn’t mean that children of people with Sjögren disease will automatically get the condition.
It’s also thought that the female hormone oestrogen could be linked to Sjögren disease, as more women get the condition than men.
How will Sjögren disease affect me?
Though the symptoms can be uncomfortable and last quite a long time, you should be able to lead the life you want if the condition is treated properly. For most people, the condition only affects the tear and saliva glands, but some people may experience other symptoms, such as fatigue and joint inflammation.
If dryness of the eyes isn’t treated, the front of your eye could become damaged and cause permanent sight problems. Seeing an optician regularly and using treatments for dry eyes can help stop this.
People with Sjögren disease might be more likely to develop:
- hypothyroidism, when the thyroid gland is underactive
- Raynaud’s phenomenon, which causes the fingers to feel cold and turn blue
- inflamed blood vessels, known as vasculitis, which can cause reduced blood flow
- loss of feeling in the hands and feet, known as peripheral neuropathy
- IBS, causing tummy pain, diarrhoea and constipation
- kidney problems
- liver problems, including a condition known as primary biliary cholangitis
- purple spots on the lower legs, known as purpura
- pleurisy, which causes chest pain and shortness of breath
- coeliac disease, which is an autoimmune condition that causes the gut to react to gluten – this is found in food such as bread, pasta and cereal.
Your doctor will look out for symptoms such as extreme tiredness, fever, lack of energy and difficulty concentrating. This may indicate that you have one of these conditions.
Occasionally, scar tissue can form in the lungs, causing breathlessness, a dry cough and chest pain. This is known as pulmonary fibrosis and requires specialist advice. However, drugs can be prescribed to treat this.
You might be more prone to lung infections, or your airways might widen, due to a condition known as bronchiectasis. See your doctor if you have a cough, wheezing or shortness of breath that doesn’t go away. Stopping smoking can also help reduce the risk of these conditions.
Lymphoma
Very rarely, people with Sjögren disease have an increased risk of developing cancer of the lymph nodes or glands. This is known as non-Hodgkin lymphoma, but only affects a very small number of people.
You and your doctor should regularly check for any early signs, such as a fever, salivary glands that are persistently swollen, and enlarged lymph glands in your neck, armpits or groin. See your GP if you notice any of the above symptoms, if you start having night sweats, or lose weight without meaning to.
Diagnosis
There are other conditions that have similar symptoms, so it can sometimes take a while for people to be diagnosed with Sjögren disease. It’s important you get an accurate diagnosis, so you can start the right treatment as soon as possible. Your doctor will ask about your symptoms and test the dryness of your eyes and mouth.
Because there are a number of possible symptoms and complications, it’s likely that you’ll also need to see an eye specialist known as an ophthalmologist (of-thal-mol-uh-jist), a dentist or oral surgeon, or a rheumatologist (roo-ma-tolo-jist) before you’re diagnosed.
What tests are there?
There are a number of tests that can help a doctor diagnose this condition.
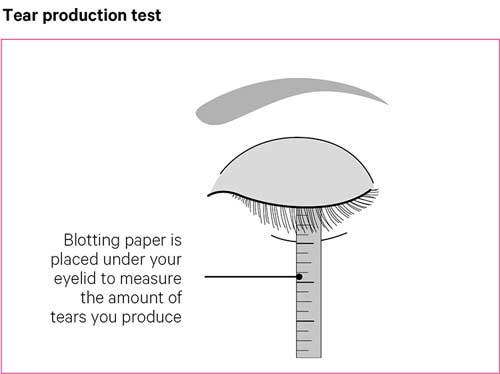
Tear production
In this test, a small piece of blotting paper is used to measure your tear production. The paper is placed in the corner of your eye and folded over your lower eyelid.
This can be a little uncomfortable and will cause your eye to water, making the paper wet. To see how good your tear production is, your doctor will measure the amount of water that soaks into the blotting paper within five minutes.
Eye examination
During this test, an eye specialist will put a dye into your eyes and use a microscope with a light to examine them.
The light makes it possible to see the film of liquid over the surface of each eye. If you don’t have enough of this liquid, you may have Sjögren disease.
Spit test
This test involves getting you to spit or dribble into a container over five minutes. The amount of saliva that you produce in that time is measured.
If it’s lower than expected, this could be a sign of this condition.
Ultrasound scans
Ultrasound scans can sometimes help with a diagnosis, with high-frequency sound waves used to build up pictures of your salivary glands.
The glands usually appear grey on ultrasound images, but in people with Sjögren disease, round black areas can be seen in the scans.
Sialography
A sialography is an x-ray of the salivary glands and ducts. In this x-ray, contrast dye is injected so that the glands and ducts show up clearly in the images.
This can be used for diagnosis, but is mainly used to identify blockages of the ducts in people who keep getting salivary gland infections.
MRI scans
Occasionally, magnetic resonance imaging (MRI) scans are used if there is uncertainty over the diagnosis, or if it is thought you may have another condition, such as lymphoma. MRI scans use radio waves in a strong magnetic field to build up pictures of the inside of the body.
Blood tests
People with Sjögren disease often have high levels of inflammation in their blood, which can be measured with blood tests, such as an erythrocyte (er-i-throw-site) sedimentation rate test. This is also known as ESR.
Two autoantibodies, called anti-Ro and anti-La, are important in diagnosis and can be found in blood tests. About two-thirds of people with primary Sjögren disease have anti-Ro or anti-La antibodies, or both.
The presence of one or more of these autoantibodies in a person with dry eyes or a dry mouth strongly suggests they have the condition. But not everyone with the condition has these autoantibodies, so your doctor may need to use other tests.
Lip biopsy
A lip biopsy is done to see if any clumps of white blood cells have formed inside your salivary glands, and might also be used to check if you’re at risk of lymphoma.
During the biopsy, a tiny piece of tissue containing several tiny salivary glands is removed from your lower lip under local anaesthetic and examined under a microscope.
"I was surprised at the diagnosis, but also relieved: at last, my symptoms had a name. The consultant very helpfully handed me an oral hygiene starter pack, a British Sjögren’s Syndrome Association leaflet and, perhaps most valuable of all, the telephone number of a lady who had set up a local Sjögren disease support group."
Treatment
There’s no cure for Sjögren disease, but the most common symptoms can usually be treated with a combination of drugs and other treatments.
Treatments for eye symptoms
If your eyes are dry and sore, lubricating eye drops can be used to keep your eyes moist and reduce any friction. You can buy these yourself from chemists.
You might need to speak to your doctor or another healthcare professional and try a few different types of eye drops, before finding one that is right for you.
For very dry eyes, you may need to use ointment, gel or sprays as well as eye drops. Your doctor might give you eye drops containing ciclosporin or steroids if your eyes are inflamed.
Mucolytic eye drops can be given by your doctor if mucus has caused your eyes to become sticky. Paraffin-based ointments can be used at night to help stop your eyes being dry and crusty when you wake up in the morning.
If you need to use eye drops more than three times a day, it’s a good idea to use a brand that is preservative-free, as regularly using eye drops that contain preservatives can increase dryness and sensitivity. If you have corneal ulcers or infections, it’s important to speak to an eye specialist before using any products.
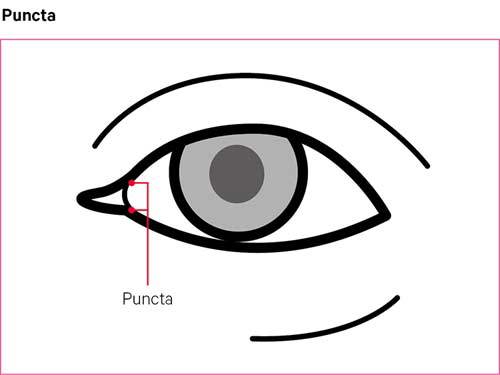
In some cases, an eye specialist may suggest punctal occlusion. This is where tiny plugs are inserted into the ducts at the inner corners of the eyelids. These are known as the puncta. This reduces the ducts’ ability to drain tears or eye drops from the surface of the eye.
Temporary plugs are usually tried first, and if these are helpful, more permanent plugs can be inserted. If the eyes remain very dry, the puncta may be sealed with heat in a procedure known as cauterisation.
Treatments for mouth and throat symptoms
If you have a dry mouth, you should try to see a dentist every three to six months, so they can monitor and treat your symptoms.
You may find that artificial saliva, lozenges, sugar-free gum or gels help your mouth feel less dry. Sprays are also good, but some are acidic and can increase tooth decay, so make sure you use ones containing fluoride.
Antifungal treatments can also help if your mouth is very dry and this is causing other problems, such as fungal infections and dry coughs. Mouth rinses containing chlorhexidine may help with your dental hygiene, but you should only use them for short periods of time every so often, as they could stain your teeth.
You can also get toothpastes or mousses containing fluoride, which can help reduce decay. Try to use alcohol-free products, as products containing alcohol can dry your mouth out.
You should be able to get most of the products above from a chemist or supermarket.
If your salivary glands are making the sides of your face painful, talk to your doctor, as you may have an infection. If it’s not an infection, you may be prescribed a short course of a steroid called prednisolone, or given a steroid injection to reduce the inflammation.
Drugs
There are a number of drugs that can be used to treat Sjögren disease.
Pilocarpine
Pilocarpine tablets, also known as Salagen, can boost the amount of saliva and tears your glands make. It might also help to reduce dryness in other areas of your body, such as the throat and vagina.
Some people do get side effects, but these normally get better over time. These can include:
- sweating
- headaches
- needing to pee more often.
It may help to start on a low dose and gradually increase it as your side effects improve.
Painkillers and NSAIDs
Painkillers and non-steroidal anti-inflammatory drugs (NSAIDs) can be used to treat joint pain and aching. They can be bought over the counter in supermarkets and chemists, but your doctor may be able to prescribe you stronger versions if you need them.
NSAIDs help to reduce inflammation and control pain, swelling and stiffness. Common examples include ibuprofen, naproxen and diclofenac. Painkillers, such as paracetamol, can also be used to treat bad headaches, alongside anti-migraine medications.
Steroids
Steroids, also known as corticosteroids, can be used to treat some of the symptoms, but they won’t change the condition itself.
If your joints are inflamed, a steroid injection or short course of steroid tablets may be suggested, as these will make you feel better straight away. If your condition is more severe, you might need to take steroids for a longer period of time.
DMARDs
Disease-modifying anti-rheumatic drugs, or DMARDs, reduce the activity of the immune system. They’re sometimes used to treat the long-term symptoms of the condition, or given to those who have a more severe type.
These drugs aren’t normally used if you only have symptoms affecting your mouth and eyes, but can be given if you have joint problems, or complications affecting your organs.
Hydroxychloroquine is the DMARD that is normally used to treat joint pain, aching and fatigue. Other DMARDs that can be used to treat the condition include:
You might be given another drug, such as colchicine or dapsone. Tacrolimus is another DMARD that can be used to treat problems with the skin, if hydroxychloroquine doesn’t help.
Rituximab is a type of DMARD known as a biological therapy, which targets the B-cells of the immune system.
It’s given to people who have other complications of Sjögren disease, such as interstitial (in-ter-stish-al) lung disease, idiopathic thrombocytopenic purpura (id-ee-oh-path-ick throm-bow-sigh-toe-pee-nick per-pure-rah) or lymphoma. It is also used when steroids and other DMARDs haven’t worked. It’s not used very widely, because it’s not currently approved for use in Sjögren disease through the NHS.
Other treatments
Drugs such as nifedipine, which open up the blood vessels, may be prescribed if you have Raynaud’s phenomenon. Antispasmodic drugs such as mebeverine can be helpful for treating tummy pain and bowel problems.
If you have vaginal dryness, you can use creams that don’t contain hormones to improve this. Ask your pharmacist for more information about this. Hormone replacement therapy (HRT) can be used if you have more severe symptoms of menopause, but it’s important to discuss the risk of side effects with your doctor.
You might be given a drug therapy known as intravenous immunoglobulin (IVIg). IVIg isn’t usually given for Sjögren disease, but if you have myositis or other linked conditions it might be used, especially if other drugs haven’t worked.
Managing symptoms
There are a number of things you can do to ease your symptoms alongside the treatments mentioned above.
Reducing your symptoms
Try making the following small changes where you can in your daily life:
- Wear wraparound sunglasses or glasses with side shields to help retain moisture in your eyes.
- Keep your eyelids and the surrounding areas clean to increase the amount of oil leaving your eyelid glands.
- Avoid places that are smoky or windy, as this could dry your eyes out.
- Use a humidifier, plants or bowls of water to increase humidity and keep the air in rooms moist.
- Have regular appointments with an optician to check the health of your eyes.
- Take regular breaks from screens – avoid using a computer, phone or the TV for a long period of time.
- Have a good dental care routine and regular check-ups.
- If you smoke, try to give up. You can get help and advice on this from NHS Smokefree.
- Avoid strong soaps if you have dry, itchy skin. Water-based creams and emollients may be helpful.
- Wear sunscreen with SPF 15 or higher if your skin is sensitive to the sun or comes out in a rash.
- Wear warm gloves if you have Raynaud’s phenomenon. Exercise will help by improving your circulation
"I do exercises and enjoy walking. When outdoors, I depend on my sunglasses with silicon eye cups."
Exercise
Exercise is really important, especially if you have symptoms in your joints.
A physiotherapist can advise you on suitable exercises and on how to increase your activity level gradually. Exercise can also help with extreme tiredness, difficulty concentrating, joint stiffness and symptoms of depression.
Diet and nutrition
There’s no special diet that’s recommended for people with Sjögren disease. However, if you have tummy pain or bowel problems, increasing the amount of fibre in your diet should help.
Your doctor may be able to refer you to a dietitian, who is trained in giving advice on diet, and they can give you support and suggestions to ease any tummy problems.
Cutting down on sweet food and drinks will help to reduce any dental problems. Keeping to a healthy weight can also help, and this will also reduce strain on your joints.
Remember that alcohol, tea, coffee and other caffeinated drinks can dehydrate you. Sipping water or sucking ice cubes regularly can help to relieve a dry mouth.
Complementary treatments
There’s no research showing that complementary treatments can ease the symptoms of Sjögren disease. Most complementary treatments generally don’t cause serious side effects in people with the condition, but you should always discuss them with your doctor before starting treatment.
There are some risks associated with specific therapies, and it’s important to go to a legally registered therapist, or one who has a set ethical code and is fully insured. If you decide to try therapies or supplements, you should consider carefully what they’re doing for you and whether you notice any improvement, before deciding to continue.
Support from others with the condition
Joining a local support group can be a good way to meet others and get useful tips for managing your condition. You might also find useful tips in online forums through related organisations, including Versus Arthritis.
"It’s great to bring people together who can offer each other support, information and advice. We all really understand each other and as it’s such a rare condition, it’s great to be able to ask someone who is going through the same thing. I’m so proud of what we’ve done creating this community.”
Related information
Living with Sjögren disease
"Sjögren disease has profoundly affected my life and that of my family. I have tried to manage over the years by changing what I do and how I do things. I gave up driving, because of light-sensitivity and because fatigue impairs my judgement and decision making."
Work
Work can provide a sense of purpose, a supportive social network, and help you financially. Some people find that continuing to work can actually help reduce symptoms such as fatigue and any mental fog.
There are rights to protect you at work in the UK, and your employer has a duty to make reasonable adjustments to enable you to do your job. The Equality Act 2010 makes it illegal to treat anyone with a long-term condition, such as Sjögren disease, worse than someone who doesn’t have a condition.
Access to Work is a scheme in Scotland, England and Wales that gives extra help to people with disabilities or physical and mental health conditions. There is a separate scheme available in Northern Ireland.
Access to Work provides funded or partly-funded grants to help people start work, stay in work, or move into self-employment, and can be used to pay for equipment, support workers, or transport, among other things.
Coping with fatigue
Fatigue is a feeling of tiredness or exhaustion. It affects people in different ways, but it can make doing daily activities hard. You might feel like your limbs are heavy and as if you have no energy.
It’s a good idea to speak to your rheumatology team about your treatment, as fatigue can be a side effect of some drugs. It can also be caused by your condition being active and causing inflammation, so they may want to look at the dose and type of medication you’re taking.
Try these useful tips to reduce your fatigue:
- Increase the amount of physical activity you do to boost your energy levels. Starting slowly, even with just a 5 or 10 minute walk, can make a difference.
- Eat a balanced diet to make sure you have all the nutrients you need to keep your energy levels up.
- Introduce relaxation techniques into your daily life to reduce feelings of stress. Listening to music, spending time with friends and exercising can all help.
- Speak to your GP, rheumatologist or friends about low mood, as this might be linked to fatigue. Talking therapies, such as counselling, have been shown to help improve low mood and fatigue.
- Plan and prioritise things you need to do and avoid leaving all the demanding jobs to do in one go. Pace yourself by breaking tasks down into smaller jobs, and take regular breaks.
Sex, fertility and pregnancy
Women with Sjögren disease can sometimes have a dry vagina, which can make sex painful. Lubricants and creams made from the female sex hormone, oestrogen, can help with this. Treatments for infections such as thrush are available from chemists.
The condition doesn’t affect fertility in men or women. However, there may be a higher risk of miscarriage in women who have anti-Ro or anti-La antibodies. Your doctor might suggest low-dose aspirin in the early stages of pregnancy to reduce this risk.
There aren’t usually any problems during or after pregnancy, and you may be able to carry on with some treatments, such as hydroxychloroquine, during pregnancy.
However, a very small number of women may pass anti-Ro or anti-La antibodies on to their baby during pregnancy. The baby could then develop symptoms, such as rashes and abnormal blood tests after birth.
These will clear up once the mother’s antibodies have been lost from the baby’s blood. This can take anything from a couple of weeks to a few months.
In some cases, the antibodies affect the baby’s heart, causing it to beat slowly. If you have these antibodies, you should tell your obstetrician, as your baby’s heartbeat will need additional monitoring in the womb.
"My employer is more than happy to let me go to any related hospital appointments, lets me use my aids for trips, and I know that on bad days I can take things at my pace without worrying."
Research and new developments
We’re funding several studies to improve understanding of Sjögren disease and develop new and more effective treatments for the condition.
In people with this condition, immune cells form structures called tertiary lymphoid organs (TLOs). We’re currently funding a study to understand why TLOs are present, and whether removing them could improve the condition.
We are also supporting research to uncover what causes lymphoma to develop in a small number of people living with the condition. This research may allow doctors to predict who will develop lymphoma, which means people can be treated early.
We’re also funding the SALRISE study, to establish whether electrostimulation of the salivary glands using a small electronic device can be used to treat a dry mouth.
This research will improve understanding and could allow new treatments to be developed.
Other organisations
Sjögren's UK
Sjögren's UK is a self-help organisation for people with Sjögren disease. The charity coordinates a network of regional support groups and publishes a quarterly magazine, Sjögren's Today.
Website: Home - Sjögren's UK
Helpline: 0121 478 1133
Sjögren's Foundation
The Sjögren's Foundation is an American charity. Its website gives free access to lots of information on the condition.
Website: https://www.sjogrens.org/