Introduction
There are three main types of investigations that can be used to further classify musculoskeletal presentations:
- imaging of bones and joints
- blood tests
- synovial fluid analysis.
Imaging of bones and joints
A plain x-ray of the affected joint is one of the most useful investigations. Changes that occur on plain x-ray can be characteristic of specific musculoskeletal diseases such as rheumatoid arthritis, osteoarthritis and gout. Most changes occur over a prolonged period and x-rays can therefore provide a useful historical record.
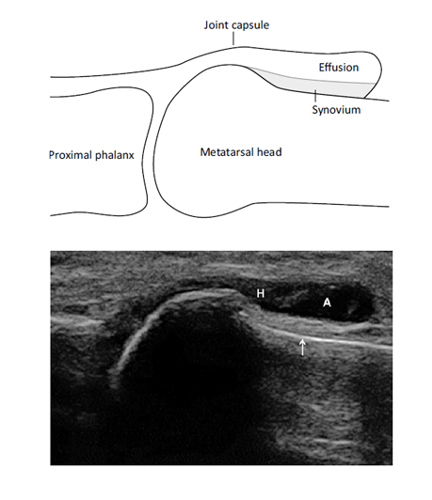
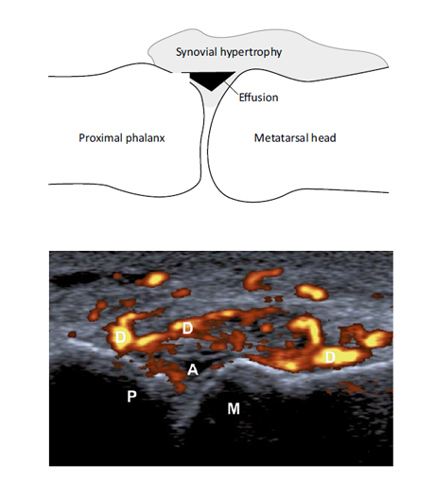
Ultrasound is becoming increasingly widely used, particularly in identifying early joint inflammation (see images below), although it doesn’t necessarily add significantly to the clinical assessment in patients with clinical signs. Other investigations – including magnetic resonance imaging (MRI), computerised tomography (CT) scanning, isotope bone scans and dual-energy x-ray absorptiometry (DEXA) scans (for osteoporosis) – all have an important role.
Grey scale scan of early osteoarthritis of the 1st metatarsophalangeal joint, showing a small anechoic effusion with some hypoechoic synovial thickening within the joint capsule. (A = anechoic effusion; H = hypoechoic synovium)
Power Doppler scan of the 1st metatarsophalangeal joint, sowing small anechoic effusion surrounded by a grade 3 Doppler signal that represents florid synovitis. (A = anechoic effusion; D = Doppler signal; M = metatarsal head; P = proximal phalanx).
Blood tests
Blood tests can be useful in indicating the degree of inflammation and in monitoring response to therapy as well as helping to achieve a diagnosis:
- The erythrocyte sedimentation rate (ESR) is one of the best-known inflammatory markers and indicates what has been happening over the last few days or longer. It is non-specific and influenced by many things including anaemia.
- C-reactive protein responds more rapidly to changes in inflammation – normally within days.
- Serum uric acid may be raised in gout, although it may be unreliable during an acute episode.
- Increased titres of a number of autoantibodies may be found, although their significance is not always clear. Tests for rheumatoid factor and anti-CCP (cyclic citrullinated peptide) antibody, for example, are both often strongly positive in patients with rheumatoid arthritis. However, rheumatoid factor may also be positive in other disease states and in the elderly and is therefore not highly specific.
It is also important to consider infection as a cause of an arthropathy, particularly in the case of a single joint – blood cultures for infection should be taken even if there is no fever.
Synovial fluid analysis
Obtaining a sample of synovial fluid for analysis is an important skill to learn and is vital to perform in order to exclude infection of a joint, which would normally present with an acute monoarthritis with systemic symptoms. Synovial fluid should be sent for culture and gram staining. If gout or other crystals are considered as a cause of the problem, the fluid is examined for crystals under a polarizing light microscope.