Examination of the hand and wrist video
Watch now
A short video demonstrating how to examine the joints of the hand and wrist.
Introduction
This should normally take place with the patient’s forearms exposed to above the elbows. The patient’s hands should be resting on a pillow as it can be painful for patients with elbow or shoulder problems to hold their hands up for long periods.
Look
With the patient’s hands palms down:
- Look at the posture and check for obvious swelling, deformity, muscle wasting and scars.
- Look at the skin for thinning and bruising (possible signs of long-term steroid use) or rashes.
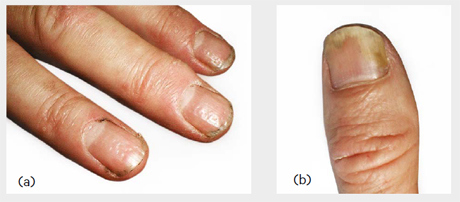
- Look at the nails for psoriatic changes such as pitting or onycholysis (see image below), and evidence of nailfold vasculitis.
- Decide whether the changes are symmetrical or asymmetrical.
- Do the changes mainly involve the small joints (PIPs and DIPs, MCPs etc) or the wrists?
It is often helpful to structure the inspection from proximal to distal to ensure that all areas are systematically assessed.
Ask the patient to turn their hands over:
- Does the patient have problems with this due to proximal or distal radioulnar joint involvement?
With the patient’s hands palms up:
- Look again for muscle wasting – if present, is it in both the thenar and hypothenar eminences? If it is only in the thenar eminence, then perhaps the patient has carpal tunnel syndrome. Look for signs of palmar erythema. Look at the wrist for a carpal tunnel release scar.
- Look at the elbow for rheumatoid nodules, psoriatic plaques and surgical scars.
Feel
With the patient’s hands palms up:
- Feel for peripheral pulses (ischaemia could be causing pain).
- Feel for bulk of the thenar and hypothenar eminences and for tendon thickening.
- Assess median and ulnar nerve sensation by gently touching over both the thenar and hypothenar eminences, and the index and little fingers respectively – if not normal and equal, this may indicate an entrapment neuropathy.
Ask the patient to turn their hands back over, so their palms are face down:
- Assess radial nerve sensation by light touch over the thumb and index finger web space.
- Using the back of your hand, assess skin temperature at the patient’s forearm, wrist and MCP joints. Are there differences?
- Gently squeeze across the row of MCP joints to assess for tenderness (watching the patient’s face for signs of discomfort).
- Bimanually palpate any MCP joints and any PIP or DIP joints that appear swollen or painful. Is there evidence of active synovitis? (The joints will be warm, swollen and tender and may have a ‘rubbery’ feel, or you may even detect effusions).
- Are there hard, bony swellings? Check for squaring of the carpometacarpal (CMC) joint of the thumb and for Heberden’s nodes on the DIPs. There may be evidence of previous synovitis (thickened, rubbery but non-tender joints).
- Compare one joint with another, or with your own, to decide whether the small joints are normal.
- Bimanually palpate the patient’s wrists.
- Finally run your hand up the patient’s arm along the ulnar border to the elbow. Feel and look for rheumatoid nodules or psoriatic plaques on the extensor surfaces.
Move
- Ask the patient to straighten their fingers fully (against gravity). If the patient is unable to do this it may be due to joint disease, extensor tendon rupture or neurological damage – this can be assessed by moving the fingers passively.
- Ask the patient to make a fist. If they have difficulty tucking the fingers into the palm, this may be an early sign of tendon or small joint involvement. Move the fingers passively to assess whether the problem is with the tendon or nerves, or in the joint.
- Assess wrist flexion and extension actively (e.g. by making the ‘prayer’ sign) and passively (see image below).

- In patients where the history and examination suggest carpal tunnel syndrome perform Phalen’s test (forced flexion of the wrists for 60 seconds) – in a positive test this reproduces the patient’s symptoms.
- Assess power of the muscles innervated by the median and ulnar nerves. This can be done by abduction of the thumb, and finger spread, respectively.
Function
- Ask the patient to grip your two fingers to assess power grip.
- Ask the patient to pinch your finger. This assesses pincer grip, which is very important functionally.
- Ask the patient to pick a small object such as a coin out of your hand or check their ability to undo buttons. This assesses pincer grip and function.