How do the hands and wrists work?
The movement and power of your hand and wrist are controlled by muscles and tendons:
- The flexor group, on the inside or front of the arm, control bending of your fingers and wrist – these pass over the front of your wrist and are held in place by a strong fibrous band called the flexor retinaculum, or carpal tunnel ligament.
- The extensors on the outside or back of your forearm allow the hand to open up.
- Small muscles in your hand (the lumbricals and interossei) allow fine movement.
The tendons in your hand are covered by a layer of synovium, the same tissue that lines your joints. The tendon and synovium are covered by a tendon sheath, which is a bit like the protective covering on the brake cable of a bicycle.
The sense of touch in your hand is supplied by two main nerves:
- Your median or carpal tunnel nerve passes under your carpal tunnel ligament and gives feeling to most of your hand (from your thumb to half of your ring finger). It also provides power to muscles at the base of your thumb.
- Your ulnar or 'funny bone' nerve gives feeling to your little finger and half your ring finger, and it powers all of the other small muscles in your hand.
There are also two arteries (radial and ulnar) that supply blood to your hand. You can feel these on the palm-side of your wrist. The radial artery (nearer your thumb) is often felt to take your pulse. The ulnar artery on the opposite side of your wrist is much more difficult to feel.
Do I need surgery?
Most people with musculoskeletal and arthritis-related problems in their hands or wrists won't need surgery. The decision whether to operate will depend on:
- how bad your symptoms are (pain or loss of hand function)
- your needs
- your response to other treatments, including drugs, splinting and exercise.
Surgery is rarely carried out to improve the look of the hands, although an improvement in their appearance may be a welcome side-effect.
You may feel nervous, stressed or scared if you’ve been told you need surgery. Finding out as much as you can about the operation and understanding the process will help you feel calmer and more in control.
Common types of hand surgery
Conditions which may be helped by surgery include carpal tunnel syndrome, trigger finger, Dupuytren’s contracture and arthritis of the base of the thumb.
Carpal tunnel release
Carpal tunnel syndrome occurs when pressure is put on the median nerve as it passes through your wrist under the carpal tunnel ligament. This results in pins and needles and numbness in your fingers. Surgery is sometimes needed to ease pressure on the nerve. This is done by splitting the carpal tunnel ligament under local anaesthetic. You probably won't need to stay overnight in hospital.
After carpal tunnel release surgery
You may need to wear a bulky bandage on your wrist and hand for a week or two after the operation. Your stitches will be removed within 10–14 days. During this time you’ll be able to use your fingers and thumb, although you should avoid heavy tasks.
It’s important to move your fingers to prevent the nerve and tendons becoming caught up in the scar tissue which may form after your operation. You should recover from the effects of surgery in less than a month, although it may take longer to get all the feeling back, especially if you’ve had carpal tunnel syndrome for a long time. In a small number of people, the scar may ache and be sensitive for some months, but this usually settles without more treatment.
Dupuytren’s contracture fasciectomy
Dupuytren's contracture is a condition caused by tissue forming in the palm of your hand and your fingers. It's often painless and may only cause only skin nodules, but it can also form bands that make your fingers curl down into your palm. You may need surgery to remove the tissue and release your fingers, although it's not always possible to make this completely better. The operation is generally performed as a day case, so you won't need to stay in hospital.
After Dupuytren’s contracture fasciectomy surgery
It’ll take two to three weeks for your skin to heal and up to 12 weeks before you have full use of your hand. You’ll be seen by a hand therapist who will start you on exercises and monitor your movement and function. A night extension splint may be made for you, although this won’t always be needed.
Trigger finger release
If you have trigger finger, the affected finger can often bend normally but becomes stuck in a curled position. This is caused by the tendon which allows your finger to bend becoming thickened, so it becomes stuck in the tunnel where the tendon enters your finger. You may need to use your other hand to help 'trigger' your finger straight – which is where the condition gets its name from.
You may be referred to a hand therapist for a splint to be made for you to stop your finger triggering while you’re using it. A local injection helps in most cases. If this fails, you may need a minor day-case operation to open the tunnel and free the tendon. You should recover in one to two weeks.
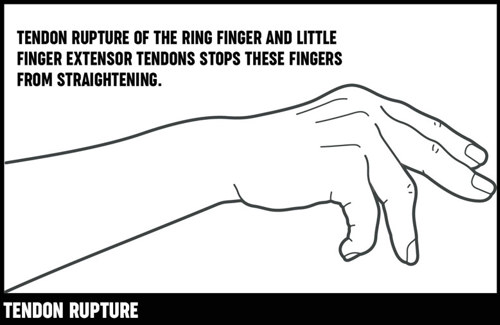
Tendon repair
There are two main groups of tendons that control your hand and wrist:
- flexor tendons, which enable you to grip and to curl your fingers into a fist
- extensor tendons, which open your fingers up.
Sometimes these tendons can tear or snap, which is called tendon rupture. Tendon rupture in your hand and wrist isn’t common, and when it occurs it’s usually as a result of rheumatoid arthritis or other types of inflammatory arthritis. You’ll need early treatment if surgery is to be successful and to protect the other tendons in your hand from rupture.
In many cases undamaged flexor tendons from other fingers are used to repair the ruptured tendon. If the tendon has ruptured because it has rubbed against rough bone in your wrist, the bone will have to be smoothed or removed to prevent the repaired tendons from rupturing again.
After the operation
Repaired tendons need at least six weeks to heal. During this time you won’t be able to use your hand at all and must only do the exercises shown to you by your hand therapist. You’ll have to wear a splint on your hand day and night to protect the healing tendons.
You’ll probably see a therapist regularly to check your finger movement and splints. It’ll be around two to three months before your hand is completely recovered.
Ganglion removal
A thick fluid called synovial fluid helps joints and tendons move slowly. Sometimes this fluid leaks out of the joint or tendon sheath. The fluid then becomes very thick and sticky, and it may form pockets of fluid (cysts) known as ganglions. These ganglions:
- feel firm or hard when pressed
- are commonly found on the back of your wrist, but they can occur elsewhere
- are commonly associated with osteoarthritis when seen on the tips of the backs of your fingers and in your wrist
Ganglions sometimes disappear on their own, but if they become painful or reduce movement the fluid can sometimes be drained using a needle. You may need minor surgery to remove them, although it's likely that they'll come back.
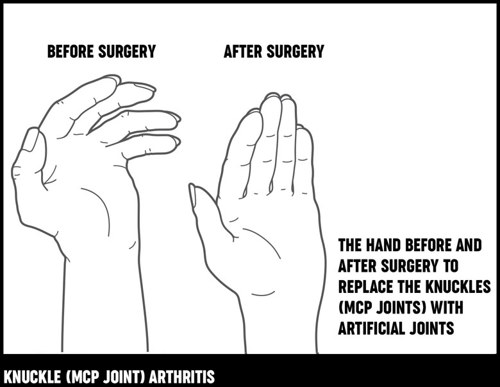
Knuckle (MCP joint) replacement
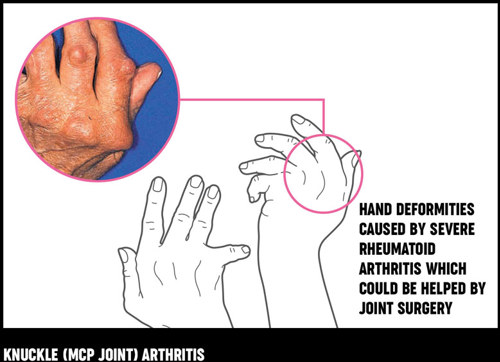
Rheumatoid arthritis of the knuckles (metacarpophalangeal or MCP joints) may cause damage and deformity, with the result that your fingers 'drift' sideways away from your thumb. This may be very painful and greatly reduce hand function. If it becomes difficult to use your hand, surgery can be carried out to replace your knuckles with small man-made (artificial) joints that act as flexible hinges. This operation reduces pain, improves the positioning of your fingers and so improves hand function.
Knuckle replacement surgery is now often performed as day surgery, although some hospitals may recommend that you stay overnight.
After the operation
After the operation you’ll have to rest your hand for a few days before you start rehabilitation. A hand therapist will teach you exercises to help you move your fingers. You should practise these at home for several months. You’ll need to wear a splint for several weeks during the day when you're not exercising, and you may need to wear it overnight for several months. Your occupational therapist can discuss ways of managing at home one-handed.
Your new joints won't be as hard-wearing as natural joints, so you'll always need to take some care when you use your hand. Your hand therapist will advise you on how to look after your new joint(s).
The MCP joint of the thumb is often affected by rheumatoid arthritis, but it’s unusual to replace it with an artificial one. Instead, the joint can be stiffened, allowing the joints next to it to make up for its loss of movement. This operation is usually effective at easing pain and improving pinching movements.
Trapeziectomy (removal of the trapezium)
Your trapezium is a bone in your wrist at the base of your thumb. If you have arthritis in the joint here, it may cause pain and make simple tasks more difficult. The pain often comes and goes, and the condition will often become painless over time. But if your pain carries on, you may need an operation to remove the joint and your trapezium.
Sometimes surgeons may make sure you can’t move your thumb/wrist for a couple of weeks to allow for scar tissue to fill the gap removing the trapezium leaves, or occasionally they use a tendon to fill the space.
After the operation
After the operation you'll be referred to a hand therapist who'll give you a splint for the base of your thumb. You'll need to wear this for six weeks. Your hand therapist will also give you exercises, which you’ll need to do for several months to get movement back and to strengthen the thumb before it feels comfortable.
Read our Trapeziectomy factsheet (PDF, 1.9 MB)
Common types of wrist surgery
Arthritis in the wrist joint is common in people with rheumatoid arthritis. Some people may need an operation if the joint is very painful and not responding to other treatment. If your wrist is badly affected, moving your hand up, down and sideways may be very painful and it’ll be very difficult to twist your forearm to place the palm of your hand upwards (this action is called supination).
The two types of wrist surgery are wrist fusion and wrist joint replacement.
Wrist fusion
Wrist fusion may be suggested if your wrist is badly damaged. This is where the bones in your wrist are fixed to the bones in your hand. This reduces pain and increases strength but usually stops you moving your wrist up and down. However, you'll probably find it easier to turn your hand.
After the operation
After the operation, you'll need to stay in hospital for a few days. You’ll need to keep your wrist protected for six to eight weeks in a lightweight cast, but your fingers will be free for light activities such as eating or writing. You may find some tasks are difficult at first but your occupational therapist will help you overcome these problems.
Wrist joint replacement
Wrist joint replacement isn't yet a common operation. The aim is to keep some wrist movement and get rid of pain.
After the operation
You’ll only be in hospital overnight but it’ll be several months before your wrist is completely recovered. Your wrist will be kept protected for two to six weeks before you start rehabilitation, which is aimed at improving the movement in your wrist and function in your hand.
Your physiotherapist or hand therapist will explain what you can and can’t do with your replacement joint and how to keep it in good condition.
Advantages
The main advantages of hand and wrist surgery can be:
- long-lasting pain relief
- better hand function
- better-looking appearance of hands
Disadvantages
There can be some disadvantages to hand and wrist surgery:
- Replacement joints, for example new knuckle joints, aren’t as hard-wearing or long-lasting as natural joints.
- You'll have scars at the site of the cut (incision).
- Some operations reduce joint movement.
- There are possible complications of surgery, for example swelling, stiffness or infection.
- Occasionally small nerves around the incision can be damaged, leading to patches of numbness.
Complications
If you’re generally healthy the risk of a serious complication from an operation is very small. Every possible care is taken to prevent complications, but in a few cases these do happen. For example, some people can develop an infection, so it’s important to speak to your doctor straight away for antibiotic treatment if you notice any signs, including:
- increased pain
- redness
- the affected area feeling warmer than usual
- an unpleasant smell
Some people may have swelling and stiffness, but physiotherapists, occupational therapists and hand therapists can help with exercises and other advice.
Bleeding and wound haematoma
A wound haematoma is when blood collects in a wound. It’s normal to have a small amount of blood leak from the wound after any surgery, and usually this stops within a couple of days. But occasionally blood may collect under your skin, causing a swelling. This can cause a larger but temporary leakage from the wound usually a week or so after surgery, or it may require a smaller second operation to remove the blood collection. Drugs like aspirin and antibiotics can increase the risk of haematoma after surgery.
Preparing for surgery
Before the operation you’ll be asked to sign a consent form, which gives your surgeon permission to carry out the treatment. It’s important to ask any questions you may still have at this stage. Ask your doctor, nurse or therapist to explain anything you don’t understand. You should also discuss with your surgeon, anaesthetist or nurse at the pre-admission clinic whether you should stop taking any of your medications or make any changes to the dosage or timings before you have your surgery. Different units may have different advice.
A doctor or nurse will check your general health to make sure there won’t be problems with a general anaesthetic if this is being used.
Read more about types of anaesthetic.
You should have a dental check-up and get any problems dealt with well before your operation. There’s a risk of infection if bacteria from dental problems get into the bloodstream.
You may need to wear splints after the operation, which can make everyday tasks difficult. It’s a good idea to make preparations before the operation. Simple things like choosing clothes with wide arms, stocking up your freezer or arranging to have some help in your home will all make it easier to manage one-handed. It’s a good idea to arrange help with transport, as you’ll probably have to attend hospital regularly to see your doctor or therapist. Your occupational therapist will be able to advise you before your operation if you have any concerns about coping at home afterwards.
Recovery
This will depend on the type of operation and your general health. Ask your surgeon what you should expect after the operation. Planning ahead can make it easier to manage when you return home.
Different surgeons have different ideas about the treatment required after an operation. This is affected by the type of operation and your health. You may need to wear splints to protect the healing tissues and bone, but you should discuss with your surgeon what to expect after the operation. Your nurse, occupational therapist, physiotherapist or hand therapist will be able to offer support.
After you’ve been discharged from hospital an appointment will be made for you to come in as an outpatient to check your progress. Sometimes your GP will help with this aftercare. A district nurse or practice nurse may be asked to remove stitches and change dressings.
If you stopped taking any of your regular drugs or had to alter the dose before the operation, it’s very important to talk to your rheumatologist for advice on when you should restart your medication.