Why osteoarthritis isn't ‘just a bit of wear and tear'
07 December 2023
Did you know that around 10 million people have osteoarthritis? This is the most common type of arthritis, which will affect half of us by the time we are 70.
Even though it affects millions, many people living with osteoarthritis are often told that it’s ‘just a bit of wear and tear.’ But that simply isn’t true.
Here we deep-dive into osteoarthritis, meet a researcher who is working tirelessly on treatments, and offer advice on how you can manage your symptoms.
It’s not ‘wear and tear’
There are a lot of misconceptions about osteoarthritis but one of the most unhelpful is that it’s ‘just a bit of wear and tear.’
The truth is our joints aren’t like car tyres that wear down and need replacing. They’re complex living tissues that our bodies constantly repair and maintain.
Osteoarthritis happens when our bodies can no longer do this effectively. So, it’s not an inevitable part of getting older. It’s an active disease process.
What happens in a joint with osteoarthritis?
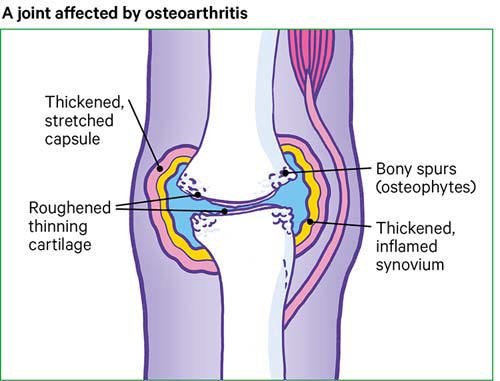 In a healthy joint, the ends of the bones are covered with cartilage. This is a coating of tough tissue that’s smooth and slippery.
In a healthy joint, the ends of the bones are covered with cartilage. This is a coating of tough tissue that’s smooth and slippery.
Cartilage allows our bones to move freely over each other. But, when a joint develops osteoarthritis, part of the cartilage thins, and the surface becomes rough. This means the joint can’t move as smoothly as it should.
When the cartilage changes in this way, the body tries to repair it. The tissues within the joint become more active than normal to try to make this happen.
Sometimes this works well. But other times, the repair process doesn’t work as it should – and this can cause further changes in your joint.
Extra bone might form around the edges of the joint (called osteophytes). Or the lining of the joint capsule called the synovium (pronounced “sye – no – vee – um”) may thicken and produce more fluid than normal, causing your joint to swell.
Changes like these can lead to pain, stiffness, swelling, or difficulty moving your joint properly. This is what we call osteoarthritis. Osteoarthritis can affect any joint in the body but the most commonly affected are the knees, hips and hands.
A glimpse of our osteoarthritis research
 Our researchers are working tirelessly to find better treatments, therapies and, hopefully, cures for arthritis – and one of these is Dr David Wilkinson, a biochemist funded by Versus Arthritis. A biochemist is a scientist who studies the chemistry of living things.
Our researchers are working tirelessly to find better treatments, therapies and, hopefully, cures for arthritis – and one of these is Dr David Wilkinson, a biochemist funded by Versus Arthritis. A biochemist is a scientist who studies the chemistry of living things.
Right now, David’s team are focusing on osteoarthritis. They’re looking at how the cartilage that coats the end of bones becomes thinned and rough in osteoarthritis.
We know that osteoarthritis:
- is an active process.
- is not 'wear and tear'.
- involves enzymes.
Enzymes are tiny protein molecules that speed up chemical reactions in the body. In this case, the enzymes are supporting a chemical reaction that breaks down cartilage.
David and his team are exploring which enzymes play an important role in joints affected by osteoarthritis. He also wants to see whether there are any medicines we could develop to target these enzymes.
“We know that the enzymes work together to breakdown the joint in osteoarthritis. It's a bit like a relay race. One enzyme will 'activate' another one. What we want to know is which enzymes are most important, and when.”
Managing osteoarthritis symptoms
Although there is no cure for osteoarthritis yet, there are treatments that can help control symptoms. Plus, there are important and achievable steps you can take to look after your joints too.
Everyone is different. So, it’s about finding what works for you.
Diagnosis, and information

Understanding your diagnosis and your options is the first step to better managing your condition. For that reason, it’s worth:
- Checking that you know your diagnosis and making an appointment if you're not sure.
- Learning more about your condition.
- Reviewing Decision Support Tools. These are questions and answers that are designed to help you make an informed decision about your treatment. You can use them to start a conversation with your doctor, talk through your options, and decide what is right for you.
Medicines and treatments
There are also medicines and treatments you can try. While these won’t slow down or reverse the changes in your joint, they should help ease pain and stiffness.
Some of these you can buy yourself from pharmacies, shops, supermarkets or online. For example, non-steroidal anti-inflammatory drugs, such as ibuprofen.
Others may need to be prescribed by your doctor. These include:
- Short term opioids, such as codeine.
- Steroid injections.
- Surgery, such as a joint replacement, if your pain is severe.
- AposHealth therapy (these are specially adapted shoes that may help with painful or stiff knees).
Managing your condition yourself
With the support of your healthcare team, there are other small steps you can take to manage your condition yourself.
Physical activity
 It can be hard to keep moving when you have arthritis. But staying as active as possible can reduce your pain and help you stay independent.
It can be hard to keep moving when you have arthritis. But staying as active as possible can reduce your pain and help you stay independent.
As well as reducing pain, exercise can:
- improve your muscle strength which keeps your joints strong and well-supported.
- reduce stiffness in your joints.
- help your balance.
- improve energy levels and feelings of tiredness.
- help you manage your weight.
- boost your mood.
75-year-old Christine has osteoarthritis in her hip, knee, neck, lower spine, hands and wrists. She took part in a physical activity class and said that afterwards “everything felt looser" and "there was some improvement in pain too."
Conserving energy (also called ‘Pacing')
 On good days, when your pain isn’t too bad, it’s easy to overdo it. But this can lead to more pain, which might eventually put you off doing daily chores or the activities you enjoy. This is sometimes described as the ‘boom and bust’ cycle.
On good days, when your pain isn’t too bad, it’s easy to overdo it. But this can lead to more pain, which might eventually put you off doing daily chores or the activities you enjoy. This is sometimes described as the ‘boom and bust’ cycle.
Tracey, 58, lives with osteoarthritis, and says that she managed her pain levels by pacing herself. This simply means balancing the activities you need to do with breaks and rest.
"Let’s say you want to weed your flower beds,” she explains. “If we're having a good day, we tend to say, ‘Right let's get stuck in’ and we’ll also try to clean the windows and hoover the floor. Then you spend the next three hours in bed.”
“Instead, plan and pace your activities. So, plan to take some weeds out of your flower bed for half an hour. Then... rest for half an hour."
Aiming for a healthy weight
If you're overweight, losing even a small amount of weight may help to ease your pain levels. This is because being overweight can put more strain on your weight-bearing joints, such as your knees or hips.
The best way to manage your weight is through eating a balanced, healthy diet and physical activity.
We know it isn’t always easy to lose weight. If you need support, the NHS Weight Loss Plan app may be a good place to start. It can help you develop healthier eating habits and motivate you to keep moving.
Use aids and adaptations
 We know that everyday tasks — such as getting dressed or cooking meals — can feel difficult when you’re in pain.
We know that everyday tasks — such as getting dressed or cooking meals — can feel difficult when you’re in pain.
If you’re struggling, it might be worth seeing if there are any gadgets or equipment that could help put less strain on your joints. These are sometimes called aids and adaptations.
Aids are equipment that help you manage everyday tasks, such as dressing, showering, cooking, walking or sleeping. They include items such as:
- shoehorns
- walking aids
- cutlery with large handles
- two-handled saucepans
- grabbing tools
- raised toilet seats.
Adaptations are changes or additions to your home to help you move around. They can include items such as:
- A fixed ramp
- automatic doors or wider doorways for wheelchair access
- baths with built-in handles
- major permanent bathroom changes, such as a walk-in bath or wet room.
Aids and adaptations can be expensive. But you may be eligible to get aids and minor adaptations worth less than £1,000 for free from your local council. This is sometimes called ‘community equipment.’ To check if you’re eligible, simply ask your council for a free needs assessment.
If you need to make a major adaption to your home which will cost over £1000, you might also be able to get financial support from your local council. This is called a Disabled Facilities Grant.
However, the support you receive may vary, depending on your eligibility and where you live.
Talking to your employer, and making adaptations as needed
 For many of us, work offers a sense of purpose and identity, as well as financial support. So, if you’re finding it difficult to manage your symptoms in the workplace, chat to your employer.
For many of us, work offers a sense of purpose and identity, as well as financial support. So, if you’re finding it difficult to manage your symptoms in the workplace, chat to your employer.
Remember that you have options and rights.
If you consider yourself to be disabled because of your arthritis and you share this information with your employer, you have special protections under the law, including protection from discrimination and the right to reasonable adjustments.
It's important to understand what they are, so that you get the right support you are entitled to. This will help you do your job to the best of your ability and better manage your condition at work.
For instance, your employer may be able to:
- make reasonable adjustments to your job
- provide support through the Access to Work scheme.
Spending time with others with your condition
Living with arthritis can be tough emotionally, as well as physically. So, don’t be afraid to talk about what you’re going through. You deserve to be heard and your friends and family will want to support you.
Sometimes chatting to people living with a similar condition can be cathartic. They’ll understand what you’re going through and might be able to offer tips and advice.
If you’re unsure who to turn to, remember you’re not alone. You could always join one of our many branches, groups, or events in your area. Alternatively, you could chat to our Helpline or online community.
If you’re struggling with your mental health and need to talk. You could also:
- Call 116 123 to talk to Samaritans, or email: jo@samaritans.org for a reply within 24 hours
- Text "SHOUT" to 85258 to contact the Shout Crisis Text Line, or text "YM" if you're under 19.
Other ways to manage your symptoms
Although evidence is weaker in these areas, some people also find it helpful to:
- Try to stop smoking, as there is some evidence osteoarthritis symptoms may be worse in people who continue to smoke.
- Try complementary and alternative therapies. These are approaches where the evidence isn’t good enough for them to be adopted in guidelines for people with osteoarthritis, such as acupuncture or nutritional supplements. These can be expensive, and only worth continuing if you’re sure they’re helping with your symptoms.
- Look at your diet. Although there are no definite foods to eat or avoid if you have arthritis, some people find that their condition is affected by what they eat. Everyone is different though, so it’s about finding what works for you.
- Use heat or cold treatments. Some people find that applying heat or cold to their joints offers a bit of relief. Reusable ice packs, hot bottles, and microwave packs may be better than expensive gels and sprays.
We’re here to help
If you’re struggling with pain and fatigue, remember you’re not alone. If you need advice or support, you can:
- Call our free helpline on 0800 5200 520
- Chat to our Arthritis Virtual Assistant
- Join our online community
- Stay in touch and follow us on X (Twitter), Facebook and Instagram.